The previous article in this series helped answered the question – What is a pressure ulcer? – as well as outlining how prevalent they are, how they develop and who is at risk of developing a pressure ulcer. In this article, we’ll be looking at answering another key question – What are the stages of a pressure ulcer? – and we’ll also look at the cost of prevention vs treatment of the various stages of pressure ulcers.
The EPUAP (European Pressure Ulcer Advisory Panel), NPUAP (National Pressure Ulcer Advisory Panel) and the PPPIA (Pan Pacific Pressure Injury Alliance) collaboratively released The International Pressure Classification System in 2009 and it was re-published in 2014 and it provides a good overview of the stages of pressure ulcers.
What are the stages of a pressure ulcer?
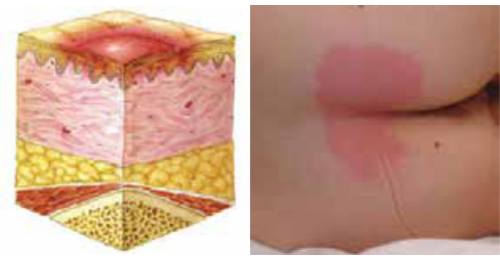
The are 4 category/ stage classifications of pressure ulcers:
- Category/Stage I: Nonblanchable Erythema
- Category/Stage II: Partial Thickness Skin Loss
- Category/Stage III: Full Thickness Skin Loss
- Category/Stage IV: Full Thickness Tissue Loss
We have outlined each of these stages in the slides below along with illustrations and example imagery. Please note, some of the imagery in the slides below may be considered graphic.
Source: Prevention and Treatment of Pressure Ulcers: Quick Reference Guide (EPUAP, NPUAP, PPPIA)
If you have a pressure ulcer
If you think you may be developing or at risk of developing a pressure sore, the next article addresses the question – How can I tell if I have a pressure sore? – however, with pressure it is best to err on the side of caution and contact your local GP, healthcare professional or medical center.
This article is part 2 of a 5-part series on pressure care and pressure ulcers to help raise awareness of pressure ulcers as part of STOP Pressure Ulcers 2019.
Click Here for Part 3 of the Series – “How to tell if I have a pressure sore?” >
Preventing and Treating Pressure Ulcers with the Star Lock Cushion
The Star Lock Cushion is one of the best pressure care cushions available for preventing and treating pressure ulcers of wheelchair users. It is clinically proven for the treatment Stage IV pressure ulcers.
Click here for more information.